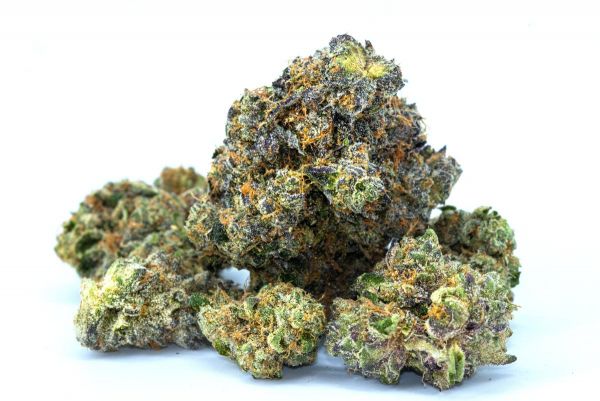
 Marijuana is increasingly legalized and accepted in the United States, but some suggest this could be increasing psychosis-related mental disorders including schizophrenia. While schizophrenia is a complex mental health disorder, heavily linked to genetics, there is significant evidence showing a potential link to cannabis use. This link is also genetic dependent, with most studies suggesting two gene expressions (AKT 1 C/C and COMT) as being largely responsible.
Marijuana is increasingly legalized and accepted in the United States, but some suggest this could be increasing psychosis-related mental disorders including schizophrenia. While schizophrenia is a complex mental health disorder, heavily linked to genetics, there is significant evidence showing a potential link to cannabis use. This link is also genetic dependent, with most studies suggesting two gene expressions (AKT 1 C/C and COMT) as being largely responsible.
If you or a loved one is using cannabis or marijuana in any form, it’s important to understand there could be a risk. This article covers the studies and known links between marijuana and schizophrenia to help you decide about the safety of using cannabis.
Cannabis and Vulnerability to Schizophrenia
Cannabis is very firmly linked to psychosis and psychotic episodes including paranoia and hallucinations. As a hallucinogenic, cannabis often interacts with dopamine and serotonin production in the brain to overload those receptors, resulting in visual and auditory hallucinations. Cannabis is very well known for side-effects like paranoia. While most people don’t link paranoia (especially mild) to psychosis and schizophrenia, an increasingly large body of science suggests it’s an important aspect. One longitudinal study of over 15,600 references showed that cannabis increases symptoms of psychosis, both in individuals with schizophrenia and those without and paranoia is one of the first symptoms.
Schizophrenia is a complex mental health disorder linked to genetics, complications during pregnancy, age of parents, and immune disorders. High exposure to psychosis and psychotic episodes may also trigger schizophrenia, but normally only when the genetic predisposition already exists. Because schizophrenia affects 0.5 to upwards of 1% of the population, with some 3+% of the population expected to be vulnerable, increased usage of psychosis-inducing drugs could increase rates of schizophrenia diagnosis and expression. This is especially critical considering some studies show that individuals who smoke cannabis are 40% more likely to have a schizophrenia diagnosis than those who do not. While there are many questions here relating to causation vs correlation (e.g., are Schizophrenic individuals more likely to show risk-taking and self-medicating behaviors and use cannabis, or is cannabis bringing out expressions of psychosis). Most evidence suggests that the actuality is a complex interplay of both factors.
How Cannabis Triggers Existing Factors
Most research strongly suggests that cannabis does not cause schizophrenia. Instead, it brings out existing genetic factors, triggering “latent” disorders. Some studies comparing individuals with and without psychosis but with a family history of schizophrenia showed that regular cannabis use results in receiving a schizophrenia diagnosis as much as 2.8 years sooner than individuals with the same family background who did not use the drug. This data is somewhat muddled by the fact that most marijuana users in the study were male, which increases risk of both using cannabis and developing schizophrenia.
Age of Use Onset – Age of first cannabis use is largely agreed as an influential factor in whether an individual develops psychosis or schizophrenia during cannabis use. Most studies show that individuals who begin using or heavily using marijuana before the age of 25 are significantly more likely to develop schizophrenia at a later age. While this may link to risk-taking behaviors associated with early-onset schizophrenia, studies suggest the relationship is much more complicated. It is most likely that there is significant interplay between the two. Individuals who smoke cannabis during their youth, when the brain is still developing, are more likely to cause permanent changes to the brain resulting in earlier onset of schizophrenia. Individuals with risk factors for schizophrenia are more likely to use cannabis and other drugs as a form of self-medication, because their dopamine and serotonin production is different from most of their peers.
Volume of Use – Heavy cannabis users develop psychosis symptoms as much as 2.7 years earlier than non-users. Light users develop psychosis an average of 2 years sooner. While there is still significant and measurable effect, it is statistically lower. However, most studies only broadly define categories of “light” and “heavy” use, with some relying solely on self-reporting. Plus, with different measures used, varying between 1 joint or less per week and 2-3 per week, for light use, larger studies with more standards across participants could be helpful in understanding the importance of volume of cannabis use. Most studies interpret “heavy” use as daily use.
Gene Expression – Genes are increasingly linked to vulnerabilities to both schizophrenia and cannabis use. Two genes, AKT 1 C/C and COMT are heavily linked to schizophrenia expression. Here, individuals with AKT 1 C/C are more than 7 times as likely to develop schizophrenia with heavy cannabis usage than any other AKT 1 expression. At the same time, individuals with the AKT 1 C/C gene are less likely than any other AKT 1 gene expression to develop schizophrenia with no cannabis consumption. Increases in schizophrenia risks are negligible to non-existent for nearly all other AKT 1 phenotypes.
COMT, the gene that regulates catechol-O-methyltransferase is another shown to increase risks of developing schizophrenia in combination with cannabis use. This enzyme degrades neurotransmitters like dopamine and norepinephrine, allowing them to be reabsorbed back into the brain. Some expression of COMT interact with cannabis in such a way that it increases degradation, greatly reducing the quantity of dopamine in the brain. Because dopamine is responsible for motivation, some emotional regulation, and anticipatory aspects of pleasure and plays a reward in the reward and processing circuit, changing levels of the neurotransmitter/hormone can dramatically change the brain.
Evaluating Risks of Using Cannabis
Today, there is a significant quantity of research into how cannabis interacts with schizophrenia and psychosis in general. Most studies strongly suggest that cannabis can play a part in psychosis and schizophrenia. Individuals who are vulnerable to schizophrenia may develop a diagnosis significantly earlier or when they wouldn’t have without using. At the same time, persons with schizophrenia are significantly more vulnerable to substance abuse, using substances as a coping mechanism, and risk-taking behavior. Cannabis usage makes schizophrenia symptoms worse, which may become permanent. This may escalate total symptoms and result in a diagnosis and anti-psychotic medication that might otherwise not have been necessary.
If you or a loved one has a family history of schizophrenia, cannabis use is likely a bad idea. Most studies indicate that very light (one dose per week) usage poses little to no risk. At the same time, people with vulnerabilities to schizophrenia are significantly more vulnerable to substance abuse and problems with controlling usage. This means you may intend to keep usage low but may have issues with moderation and maintaining a low intake. If you’re not sure, don’t know if your family has a history of psychosis, or are otherwise uncertain, there are other symptoms you can look for. For example, individuals who show paranoia when “high” are significantly more likely to have or to develop schizophrenia than those who do not.
Please be sure to consult with your doctor before deciding how to approach any drug use, and how it might affect your mental health..
And if you are struggling, it’s important to seek out professional help in the form of therapy, whether through outpatient or inpatient therapy. Many people will benefit from gender-specific mental health treatment, meaning a women’s mental health treatment program or men’s mental health treatment program. The goal is to help you identify the underlying causes behind mental illness, behavior patterns contributing to symptoms, and coping mechanisms, so that you can create new behavioral patterns and coping mechanisms, understand the root of mental illness, and build a better life for yourself. Call (800) 931 9884 for Help Today.